Resident Readiness General Surgery (61 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

5.
Are there any risks to using steroids perioperatively?
PERIOPERATIVE CORTICOSTEROIDS
Answers
1.
In patients who are glucocorticosteroid dependent, insufficient amounts of corticosteroids or cortisol resistance during critical illness may lead to secondary adrenal insufficiency with eventual hypotension, shock, and death. The patho-physiological mechanism for this hypotension cascade is not entirely clear, but is likely due to enhanced prostacyclin production and its subsequent vasodila-tory effects leading to hypotension and shock.
2.
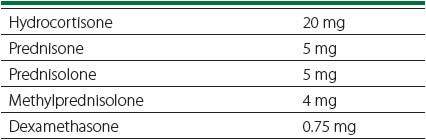
As a general rule of thumb, any patient who has received at least 20 mg of prednisone or its glucocorticoid equivalent (see
Table 46-1
) for greater than 5 days is at risk for hypothalamus–pituitary–adrenal (HPA) axis suppression. Inhaled glucocorticoids may or may not cause HPA suppression. Patients who are on lower dosages of glucocorticoids may require at least a month to develop HPA suppression. Following tapering of glucocorticoid therapy, it may take patients a year or longer to resume normal HPA axis responses with pituitary function being the first to normalize. If you are uncertain and time permits, these patients are often referred to an endocrinologist for an ACTH stimulation test to see if they secrete normal amounts of cortisol in response to ACTH.
Table 46-1.
Equivalent Dosages of Glucocorticosteroids
Because this patient was chronically on 30 mg of prednisone, he should receive stress dose steroids postoperatively.
3.
Although the actual incidence of adrenal insufficiency due to lack of exogenous glucocorticoids is likely low, it is a highly preventable cause of morbidity/mortality.
The risk of secondary adrenal insufficiency in glucocorticoid-dependent patients is directly related to the duration and severity of the surgical procedure. Relatively minor procedures that are less than 1 hour long or can be done under local anesthetic have a low degree of physiological stress. A dose of hydrocortisone of 25 mg or its equivalent is a sufficient “stress dosage” for minor procedures. For moderate-stress procedures such as peripheral bypass surgery or a straightforward small bowel resection and anastomosis a dose of 50 to 100 mg of hydrocortisone should be given intravenously prior to or at the time of skin incision. Finally, for high-stress procedures such as a total proctocolectomy or cardiac bypass procedure, a stress dose of 100 mg of hydrocortisone should be given at the start of the procedure.
4.
For minor procedures, the patient should take his or her normal dosage of steroids the morning of surgery and then resume the normal home dosage postoperatively. For moderate-stress procedures, patients should receive 25 mg of hydrocortisone intravenously every 8 hours for 24 hours and then rapidly taper to the home dosage. For high-stress procedures, patients should receive around 50 mg of hydrocortisone intravenously every 8 hours after the initial stress dose for the first 2 to 3 days after surgery and then taper dosage by half each day until you reach the home dosage.
5.
Patients who receive steroids perioperatievly are at increased risk for delayed wound healing (increased friability of the skin and vessels), infectious complications (anastomotic leak, abscess, superficial surgical site infections, etc), and gastrointestinal hemorrhage (an antacid protocol is a customary adjunct) with resulting increased length of hospitalization and need for readmission. Also, there is a normal leukocytosis with steroid administration, which may disguise normal markers of infection (fever, tachycardia, abdominal pain, etc). Finally, it is important to remember that hydrocortisone has mineralocorticoid activity at dosages above 100 mg, which can lead to unwanted fluid retention/edema and hypokalemia. Therefore, if large dosages of hydrocortisone are required beyond the initial stress dose, it is wise to use methylprednisolone as it lacks any mineralocorticoid activity.
TIPS TO REMEMBER
Any patient who has been on 20 mg or more of prednisone (or its corticosteroid equivalent) for 5 or more days should be considered to receive “stress dose” steroids prior to any procedure more complicated than an in-office “minor” procedure.
These stress dose steroids can cause significant postoperative complications and should be weaned to chronic dosage levels within 48 hours post surgery.
COMPREHENSION QUESTIONS
1.
Which patient is most
un
likely to have perioperative acute adrenal insufficiency?
A. A 40-year-old woman taking 5 mg of prednisone daily for the last year for her rheumatoid arthritis
B. A 20-year-old man taking 20 mg of prednisone daily for the last 2 weeks for a recent Crohn’s flare
C. A 55-year-old woman who has received 40 mg of prednisone daily for the last 3 months to control her recently diagnosed autoimmune hepatitis
D. A 67-year-old man taking high-dose inhaled corticosteroids for his COPD
2.
Which of the following is the correct “stress dosage” of hydrocortisone intravenously for a patient undergoing a right hemicolectomy (to be given just prior to surgery)?
A. 5 mg of hydrocortisone
B. 25 mg of hydrocortisone
C. 100 mg of hydrocortisone
D. 200 mg of hydrocortisone
3.
How long should “stress dose” steroid levels be given postoperatively?
A. Less than 3 days
B. For 5 days postoperatively
C. For 10 days postoperatively
D. Until the patient has completely healed his or her surgical wounds
4.
A patient is POD #1 from a CABG and is receiving 50 mg of hydrocortisone every 8 hours. The patient is at risk for all of the following complications secondary to the hydrocortisone
except
?
A. Hypothyroidism
B. Hypokalemia
C. Sternal wound infection
D. Leukocytosis
Answers
1.
A
. Patients taking less than 20 mg of prednisone daily (or its corticosteroid equivalent) are unlikely to develop perioperative acute adrenal insufficiency.
2.
C
. A right hemicolectomy would be considered a “moderate-stress” procedure, so 100 mg of hydrocortisone is more than an adequate stress dosage.
3.
A
. Stress dosage levels can be rapidly titrated down to home corticosteroid dosage levels within 48 hours postoperatively.
4.
A
. Hypothyroidism is not a recognized complication of hydrocortisone therapy.
 A 65-year-old Man With Diabetes Needing Postoperative Orders
A 65-year-old Man With Diabetes Needing Postoperative Orders
Roy Phitayakorn, MD, MHPE (MEd)
You are taking care of a 65-year-old man with Type 1 diabetes, which is well controlled using an insulin pump. Unfortunately, he was recently admitted with his second attack of diverticulitis and is now on your service for an elective sigmoidectomy. His surgery is uncomplicated, but now you have to write his postoperative orders.
1.
Is glycemic control really that important for patients after surgery? Why or why not?
2.
What types of insulin does a surgical patient require?
3.
How would you handle the insulin requirements of this Type 1 diabetic?
4.
What if the patient is a Type 2 diabetic who uses insulin at home?
5.
What if the patient is a Type 2 diabetic who is non–insulin dependent at home, but now requires insulin as an inpatient to maintain proper glycemic control?
PERIOPERATIVE INSULIN
Answers
1.
Diabetes is very common in hospitalized patients and inpatient hyperglycemia has been associated with an increase in overall infection rate, morbidity, mortality, and length of stay in surgical patients. These complications are probably because hyperglycemia triggers phagocyte and endothelial cell dysfunction, as well as increased vascular inflammation, platelet activation, and oxidative stress. Exogenous insulin administration not only decreases blood glucose levels but may also have a direct anti-inflammatory effect on vascular endothelial cells. However, overaggressive glycemic management can lead to hypoglycemia with possible coma, neurological injury, and death. In short, while hypoglycemia is more dangerous than hyperglycemia, both are bad. Therefore, it is essential that you understand how to properly manage perioperative insulin dosages.
2.
In broad terms, the easiest way to think about insulin requirements is the concept that inpatients require a basal or baseline amount of insulin and then a prandial or nutritional requirement (see
Figure 47-1
). The baseline amount is the quantity of insulin that patients need to avoid unchecked gluconeogenesis and ketogenesis. The prandial amount is the quantity of insulin needed to cover meals, dextrose in intravenous fluids, enteral feeds, and/or TPN. If the patient is eating, then ideally the prandial amount is given as a correction-dose therapy
before or between meals. Sliding insulin scales are substandard for this purpose since the dosage of insulin is given without regard to meals and after hyperglycemia has already occurred. If the patient is NPO and on a continuous infusion of intravenous fluids that contain dextrose, then sliding insulin scales may be sufficient to cover nutritional insulin requirements, although they should be adjusted daily until optimal glycemic control is achieved.
Other books
The Forgetting by Nicole Maggi
La gran caza del tiburón by Hunter S. Thompson
Miss Jane's Undoing by Jiwani, Sophia
Divine Madness by Melanie Jackson
Mr Palomar (Vintage Classics) by Italo Calvino
Jo Goodman by My Steadfast Heart
Black Butterfly by Mark Gatiss
In the Last Analysis by Amanda Cross
French Roast by Ava Miles
The Key by Sara B. Elfgren & Mats Strandberg
