Resident Readiness General Surgery (46 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

2.
What is your next step in the management of this patient?
3.
What blood pressure should be your goal for treatment?
4.
List three medications that you could use to treat the patient’s HTN.
POSTOPERATIVE HYPERTENSION
Answers
1.
Postoperative HTN is a sympathetically mediated response that creates vasoconstriction and increased blood pressure. If left untreated, the acute rise in blood pressure can lead to endothelial injury and end-organ damage—hypertensive emergencies. These include neurologic (ie, hemorrhagic stroke, cerebral ischemia), cardiac (ie, ischemia/infarction), and surgically related problems (ie, failure of vascular anastomoses, surgical site bleeding). No absolute BP threshold exists for the occurrence of end-organ damage, and sometimes it is the rate of increase in BP that dictates organ damage.
It is critical to consider postoperative HTN in terms of increased afterload. Acute HTN in patients with coronary artery disease (CAD), left ventricular dysfunction, and/or congestive heart failure (CHF) can be very serious. Increased afterload increases myocardial oxygen demand. This can lead to myocardia ischemia/infarction in patients with underlying CAD and limited
oxygen supply. In patients with left ventricular dysfunction the acute increase in afterload is poorly tolerated by the heart, leading to worsening CHF and pulmonary edema.
There are multiple possible reasons why a patient can become acutely hypertensive from vasoconstriction following surgery. These include:
A. Pain and anxiety: When a patient is in pain and/or is anxious, his/her sympathetic nervous system is activated, leading to tachycardia, peripheral vasoconstriction, and therefore HTN.
B. Urinary retention: A common occurrence in postoperative patients (particularly males) that can lead to significant HTN if left untreated. The mechanism is partly related to the pain/discomfort caused by bladder distension.
C. History of HTN: This is a major risk factor for developing postoperative HTN. Patients with poorly controlled HTN are at particular risk. Additionally, patients who do not take their normal blood pressure medications prior to surgery are likely to develop HTN postoperatively. (This is common because patients who follow instructions to remain “NPO” will often avoid both food and their pills.)
D. Volume overload: Patients often receive a large volume of IV fluids during surgery, particularly in prolonged cases. The resultant volume overload can precipitate HTN postoperatively.
E. Hypothermia: This leads to peripheral vasoconstriction and HTN. Patients who are not adequately covered with blankets and kept warm in the immediate postoperative period can suffer from this.
F. Hypercarbia: This is typically due to hypoventilation in the immediate postoperative period (ie, the somnolent patient lacking respiratory drive) and can lead to blood pressure elevation.
G. Type of surgery: Vascular surgery (ie, carotid, abdominal aortic), cardiothoracic, and head/neck surgery are known to predispose toward postoperative HTN.
2.
After noting that the patient has no neurologic or cardiopulmonary symptoms (ie, headache, vision changes, chest pain, shortness of breath), and before initiating antihypertensive pharmacotherapy, consider two common and easily treatable causes of postoperative HTN:
pain/anxiety
and
urinary retention
. It would be a shame to load up a patient with antihypertensive agents only to find out that the main reason for his/her HTN was an inability to void! Suprapubic fullness and discomfort on palpation, along with documentation that the patient had not voided since before surgery, would suggest urinary retention. If you are unsure, perform a bladder scan (quick, easy, and noninvasive) to confirm your suspicion.
In this patient, managing his pain with additional or alternative narcotic pain medication and assessing for urinary retention are appropriate first steps. If urinary retention is confirmed, then bladder catheter insertion is indicated. In some patients this can dramatically improve the blood pressure without ever having to give medication!
3.
The goal in managing postoperative HTN is to avoid the potentially harmful consequences described above, while also not overshooting on blood pressure decrease. There is no absolute value for a blood pressure goal. When determining your goals of treatment, consider the following:
A. Baseline blood pressure: Find out the patient’s blood pressure preoperatively. While it may seem intuitive to rapidly bring a patient’s blood pressure down to “normal” (ie, 120/80), that may not be his/her baseline. If the patient’s blood pressure is typically 150 to 160/90, then a BP of 110 to 120/50 would be low for him/her and put the patient at risk for coronary ischemia (relative hypotension, especially diastolic hypotension, leads to diminished coronary perfusion pressure and decreased oxygen delivery).
B. Rate of blood pressure decrease: The rate of blood pressure lowering is just as critical as the absolute value you aim for. Precipitous drops in blood pressure can lead to diminished end-organ perfusion.
As a general guideline, aim to reduce the blood pressure by approximately 15% in the first hour of therapy. Aim to reduce the blood pressure by
no more than 25%
over several hours.
C. Type of surgery: Postoperative HTN can be a very serious problem after certain operations (ie, vascular surgery where an anastomosis is strained by elevated intraluminal pressure and wall tension, and cardiac surgery where the recovering heart experiences a higher afterload). Compared with noncardiac surgery patients, cardiac surgery patients should be treated more aggressively to maintain a BP less than 140/90. Knowing the type of operation and any salient operative details (eg, a tenuous vascular anastomosis) is important for guiding how aggressively you try to lower a patient’s BP. Often in these types of surgery you will be given a specific blood pressure range to maintain, and this should be followed in the setting of postoperative HTN.
The presented patient’s past medical history is notable for HTN, for which he takes a β-blocker at home. He told you that his normal blood pressure is in the 130s and that he took his metoprolol the morning of surgery. Given his current BP in the 190s, and that he has undergone a low-risk operation, your target SBP should be in the 160s in the first hour, and the 140s over several hours. A β-blocker—which you know he tolerates—would be a good choice if he needs pharmacotherapy. See
Figure 36-1
for a useful algorithm.
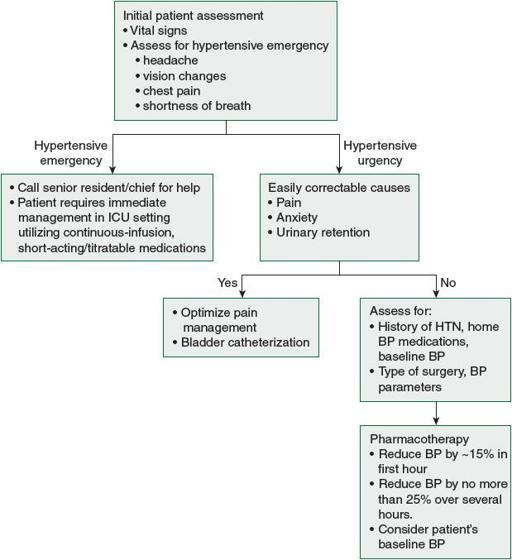
Figure 36-1.
Algorithm for approach to patients with postoperative hypertension.
4.
There are several medications used to treat postoperative HTN. There is no consensus on the “best” agent. Each has advantages and drawbacks. Three of the
more commonly used medications are
labetalol
,
nitroglycerin
, and
hydralazine
. These are described as follows and summarized in
Table 36-1
:
Table 36-1.
Pharmacologic Options for the Acute Treatment of Hypertension
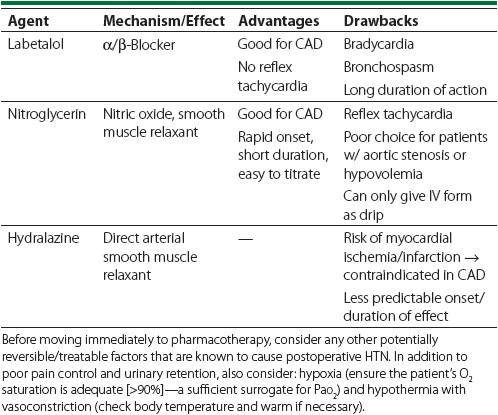
A. Labetalol: Labetalol is an α-receptor and nonselective β-receptor blocker. It blocks vasoconstriction (α) and reduces inotropy and chronotropy (β). These actions reduce blood pressure and prevent reflex tachycardia. It is therefore a good agent for patients with CAD; they would benefit from afterload reduction as well as reduction of myocardial oxygen demand to prevent ischemia. While preventing reflex tachycardia can be advantageous, the negative chronotropic effect limits its use in patients with low-normal HR (ie, 50-60 bpm). Additionally, because it is a nonselective β-blocker, it can produce significant bronchospasm in patients with reactive airway disease. Its longer duration of action (3-5 hours) also can be problematic. IV form: dose—10 to 20 mg bolus, and then 10 to 40 mg every 10 minutes (can be given as continuous infusion in the ICU setting). Onset: within minutes. Duration: 3 to 5 hours.
B. Nitroglycerin: A vascular smooth muscle relaxant (veinsarteries). Acts via release of nitric oxide. Relaxation of the vascular smooth muscle of the venous system increases venous capacitance and decreases preload. As a result, cardiac output and hence BP goes down. Nitroglycerin is another good agent for hypertensive patients with CAD who are at risk for myocar-dial ischemia. The smooth muscle relaxant effect enhances coronary perfusion; the decreased cardiac preload decreases myocardial oxygen demand. Additional advantages are its rapid onset and short duration of action—making it easy to titrate. There are several potential drawbacks of nitroglycerin. Since preload is reduced by nitroglycerin, patients who are “preload dependent” can experience dramatic, life-threatening blood pressure drops. This includes patients who are hypovolemic and those with aortic stenosis. Additionally, the decreased preload can lead to a “reflex tachycardia,” especially
in hypovolemic patients. Nitroglycerin can also cause headaches due to its vasodilatory effects. Lastly, while nitroglycerin comes in many different forms, it is the IV form that is typically used for perioperative HTN. The IV form must be administered as a continuous infusion, and therefore requires closer monitoring (ie, in the ICU). IV form: dose—5 to 300 μg/min. Onset: <1 minute. Duration: 5 to 10 minutes.
C. Hydralazine: A direct arterial smooth muscle relaxant, leading to decreased systemic vascular resistance (SVR) and blood pressure. This medication is ubiquitously used among interns and residents. However, this practice pattern is not supported by data. In fact, there are several risks with using hydralazine. Because of its effect on SVR, reflex tachycardia and increased cardiac output occur. Overall, the increased work by the heart without concordant increase in coronary blood flow puts the heart at risk for ischemia and infarction. This drug is therefore contraindicated in patients with known CAD or suspected ischemia. Another major drawback of hydralazine relates to its pharmacodynamics. IV hydralazine has a delayed onset and prolonged duration of action—not ideal when managing an acute condition. IV form: dose—5 to 20 mg q6h. Onset: 15 to 30 minutes. Duration: 4 to 6 hours.
TIPS TO REMEMBER
When assessing a patient with postoperative HTN, first assess vital signs and for the presence of end-organ damage (neurologic, cardiopulmonary). Second, look for easily treatable/reversible causes of HTN (pain, urinary retention).
Other books
On the Edge by Mari Brown
A Girl Like Me by Ni-Ni Simone
The Forever Hero by L. E. Modesitt, Jr.
Attack of the Tagger by Wendelin van Draanen
Rayuela by Julio Cortazar
The Anybodies by N. E. Bode
The CleanSweep Conspiracy by Chuck Waldron
Through the Storm by Maureen Lee
Riven (The Arinthian Line Book 2) by Sever Bronny
The Black Russian by Alexandrov, Vladimir
