Resident Readiness General Surgery (50 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

2.
C
. Female gender is the greatest risk factor.
3.
C
. This “frail” patient is at high risk of aspiration, the most likely diagnosis is ileus, and he has already vomited twice and so will most likely do so again. All 3 of these are independent reasons to place an NG tube, and a KUB would not change your management. But before you go ahead and perform this invasive procedure you should always make sure to notify your senior resident or attending.
 A 79-year-old Man, Postoperative Day 3, Who has Not had a Bowel Movement in 4 Days
A 79-year-old Man, Postoperative Day 3, Who has Not had a Bowel Movement in 4 Days
Anne-Marie Boller, MD and Joel M. Sternbach, MD, MBA
You are called to the bedside of a 79-year-old male patient for evaluation of his altered mental status. The patient is a nursing home resident, now POD 3 from a right total hip replacement, with complaints of abdominal distention and diffuse crampy abdominal pain for two days. There is no record of him having had a bowel movement since being admitted from his nursing home four days ago. A review of the patient’s medication list reveals the addition of acetaminophen/hydrocodone for pain control. He was started on a general diet and his home verapamil, furosemide, and clonidine today but was not given any of his home over-the-counter medications (including Miralax and Metamucil). There is no nausea or vomiting, vital signs are WNL and stable, and the patient has adequate urine output. He is passing flatus on a regular basis. On examination, his abdomen is distended but soft and mildly tender to palpation diffusely.
1.
What should be included in the initial evaluation of this patient?
2.
What additional testing (labs, imaging) could help guide your management?
3.
What are your options for treating constipation? Given their mechanisms, which would you choose for this patient?
4
.
You are concerned that the patient might have a fecal impaction. How do you diagnose and treat this condition? What prophylactic measures could have been taken to prevent this?
CONSTIPATION
Constipation as described by individual patients varies widely but is generally defined by decreased frequency (less than 3 bowel movements per week) and/or symptoms such as straining, passage of lumpy or hard stool, sensation of blockage or obstruction, need for manual assistance (digitations or splinting), and sensation of incomplete evacuation (in >25% of stools).
Rome III criteria provide some standardization when enrolling patients in clinical trials.
Rome III Criteria for Functional Constipation
Diagnostic criteria (criteria fulfilled for the past 3 months with symptom onset at least 6 months prior to diagnosis):
1.
Must include 2 or more of the following:
A. Straining during at least 25% of defecations
B. Lumpy or hard stools in at least 25% of defecations
C. Sensation of incomplete evacuation for at least 25% of defecations
D. Sensation of anorectal obstruction/blockage for at least 25% of defecations
E. Manual maneuvers to facilitate at least 25% of defecations (eg, digital evacuation, support of the pelvic floor)
F. Fewer than 3 defecations per week
2.
Loose stools are rarely present without the use of laxatives.
3.
Insufficient criteria for irritable bowel syndrome.
At-risk populations include the elderly, especially hospitalized or nursing home residents, and women, who are diagnosed 3 times more commonly than men. A western diet, low in dietary fiber, and inadequate fluid intake combined with prolonged immobility or a generally sedentary lifestyle all contribute to the development of constipation.
Other common causes of constipation include:
1.
Medication side effects:
A. Opiates—slow transit causing increased desiccation of stool
B. Antihypertensives, especially calcium channel blockers (verapamil)
C. Diuretics (furosemide)
D. Anticholinergics (including antihistamines and many antidepressants)
E. Iron supplements
F. Antacids with calcium or aluminum, calcium supplements
G. Antidiarrheal agents
H. Long-term laxative use/abuse
I. NSAIDs
2.
Medical conditions:
A. Hypothyroidism
B. Diabetes
C. Lupus
D. Scleroderma
E. Spinal cord injury
3.
Structural abnormalities:
A. Prior abdominal surgery causing adhesions
B. Pregnancies or history of obstetric surgery
C. Colonic stricture due to cancer, IBD, or radiation exposure
Answers
1.
The evaluation of the patient should start with a comprehensive history, focusing on establishing the onset and duration of symptoms. Constipation can be the first symptom and/or accompanying symptom of a bowel obstruction. Bowel obstructions must be thought of as organic in origin or functional in origin. Organic causes typically present acutely and can indicate the need for early imaging:
1.
Hernia
2.
Colorectal cancer
3.
Diverticulitis
4.
Sigmoid or cecal volvulus
5.
Adhesions
6.
Fecal impaction
7.
Foreign body
Functional causes are typically more chronic and warrant a more extensive outpatient evaluation:
1.
Normal-transit constipation
2.
Slow-transit constipation
3.
Outlet obstruction/constipation (pelvic floor dysfunction)
Alarm or “red flag” symptoms in addition to constipation include acute onset, nausea or vomiting, fever/chills, change in stool quality (caliber or consistency), inability to pass flatus (obstipation), severe abdominal pain and distention, unintended weight loss (>10 lb), rectal bleeding or melena, unexplained iron-deficiency anemia, or age >50 years with no prior screening for colorectal cancer with or without a family history of colon cancer. These “red flag” symptoms must be reviewed in the historical examination; they may indicate an organic cause for the patient’s constipation.
After the history is complete, a thorough physical examination should include an assessment of the patient’s general clinical condition and review of vital signs and should focus on an abdominal examination. All abdominal examinations should assess for distention, tenderness, or tympani, rule out hernias or masses, and evaluate for signs of peritonitis. Bowel sounds are generally decreased in
slow gut transit and increased or high-pitched in obstruction. External examination of the perianal region can identify anal fissures, hemorrhoids, abscesses, or protruding masses. Results of a digital rectal examination should include the following:
1.
Description of the amount and consistency of stool in the rectum
2.
Palpation for rectal masses
3.
Identification of gross blood or stool leakage
4.
Testing of the ability to contract/relax the anal sphincter voluntarily
2.
Laboratory evaluation should include a complete blood count and basic chemistry panel to screen for anemia and identify hypomagnesemia, hypercalcemia, and hypokalemia. Thyroid function tests for suspected hypothyroidism and serum lead and iron levels are also useful in evaluating the patient.
Early imaging may be considered in demented or delirious patients with constipation, as the history and physical examination may not be adequate to rule out obstruction. Plain films (KUB or acute abdominal series) may reveal megacolon or megarectum in patients with stricture or obstructing mass and can delineate the extent of fecal impaction. Evidence of bowel obstruction and perforation may also be obvious on plain films (see
Figure 39-1
).
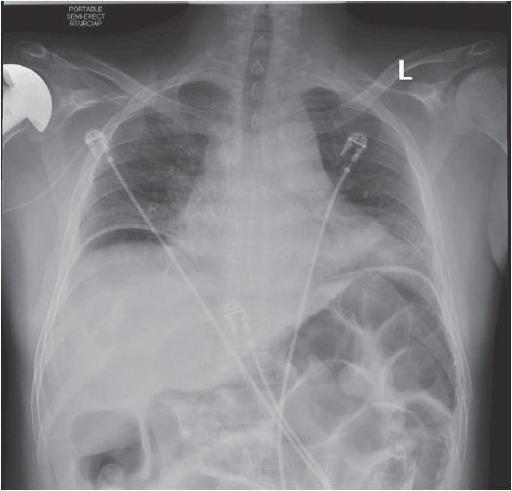
Figure 39-1.
Plain film with dilated loops of bowel and, more ominously, free intraperitoneal air.
A water-soluble contrast enema with Gastrografin (diatrizoate meglumine) or Hypaque (diatrizoate sodium) can pass an impacted area and evaluate for a more proximal mass, stricture, or perforation. It can also be therapeutic in cases of fecal impaction.
A CT scan will assist in evaluation of any obstructing mechanical or inflammatory process. If these have been ruled out, it is most efficacious to get the patient’s colon cleared of fecal debris and perform a colonoscopy, but this is not always possible in the patient with functional constipation.
3.
The first step in almost all patient populations is optimizing modifiable dietary and lifestyle factors. These include:
1.
Increasing dietary fiber to a goal of 20 to 30 g daily
2.
Ensuring adequate fluid intake with at least 6 to 8 glasses (1.5-2 L) of water daily
3.
Encouraging ambulation/regular exercise
4.
Correcting underlying electrolyte/metabolic abnormalities (and determining their cause):
A. Hypokalemia
B. Hypomagnesemia
C. Hypercalcemia
D. Hypothyroidism
E. Hyperparathyroidism
F. Hyperglycemia (DM)
G. Uremia
5.
Reviewing all medications for their constipation effects
6.
Reviewing all past and current medical/surgical problems for their possible constipating effects
After optimizing dietary, lifestyle, and behavior factors, medications can often be helpful in addressing the problem of functional constipation. There are many different mechanisms and types of laxatives that are utilized in the treatment of constipation:
