The Ins and Outs of Gay Sex (6 page)
Read The Ins and Outs of Gay Sex Online
Authors: Stephen E. Goldstone

CHAPTER
2
Common Anorectal Disorders—
OR PROBLEMS EVEN
STRAIGHT MEN HAVE
H
e lay on the emergency room stretcher, his face so pale that it was difficult to tell where the sheet ended and he began.
“You’re a very lucky man,” I said.
“Passing out is a very serious problem.
It’s a good thing your roommate found you.”
He looked away and said nothing.
“How long had you been bleeding?”
I asked.
He shrugged.
“Couple of days, but only when I moved my bowels.”
I didn’t believe him.
He had lost half of his blood, and that didn’t happen so quickly, not from hemorrhoids.
“You should have seen a doctor the moment it started.”
“I told you it wasn’t so bad.”
I patted his shoulder.
Maybe he’d talk later.
“I’m admitting you to the hospital so we can watch your blood count.
Make sure you don’t need a transfusion.”
I was almost out of the room when he said, “You’re not putting down that I was bleeding from my butt, are you?”
“Rectal bleeding from hemorrhoids.
That is your diagnosis.
I have to be honest.”
He bolted upright.
“Insurance forms go to my job.
They’ll know I’m gay.”
At some point in their lives, over 50 percent of all Americans suffer from anorectal disorders.
Because far less than half of our nation’s population is gay, we can safely conclude that most people with these problems did not get them through sex.
When a gay man develops rectal bleeding or pain, he often incorrectly attributes it to anal sex.
This is a dangerous assumption, since it often causes men to delay seeking treatment due to embarrassment and/or fear of instant “outing.”
Anal sex certainly can cause injury, but this is more often the exception than the rule.
Let me set the record straight (no pun intended):
Straight men have hemorrhoids too.
And no, your doctor cannot tell from a simple rectal exam that you’ve been fucked.
The first sign of an anorectal disorder is often a spot of bright-red blood on the toilet paper or in the bowl after a bowel movement.
The bleeding may or may not be associated with pain.
The entire bowl can even turn red.
Although frightening, this does
not
mean that you are hemorrhaging to death.
It takes only two drops of blood to turn all the water red.
If you see red water, place a tissue against your anus and be sure that the blood keeps dripping before you play drama queen and call for an ambulance.
In most cases, after your bowel movement has passed, your anus contracts and creates enough pressure to stop any bleeding.
If you follow the simple guidelines set forth in this chapter, most minor anorectal problems can be treated at home without a physician.
Of course, if your symptoms do not resolve in a day or two, if they worsen, or if other troubling signs, such as fever or purulent (infected-looking) discharge, arise, seek medical attention immediately.
Millions of years ago humans began to walk upright … and got hemorrhoids.
A slight exaggeration?
Perhaps, but
they are mentioned as far back as the Bible and in ancient Greek writings.
Many scholars believe that Alexander the Great suffered from hemorrhoids (and also that he was gay, but we won’t go there).
Napoleon had them and so did President Jimmy Carter.
Although Hippocrates performed a hemorrhoidectomy more than 2,000 years ago, most often surgery can be avoided.
Essentially hemorrhoids are varicose veins of the anus and rectum.
Hemorrhoids begin as normal veins present at the end of the rectal canal that act as cushions to ease the passage of stool.
When these small veins become abnormally dilated, hemorrhoids form.
Hemorrhoids are divided into two types:
internal and external.
(See
Figure 2.
1
.
)
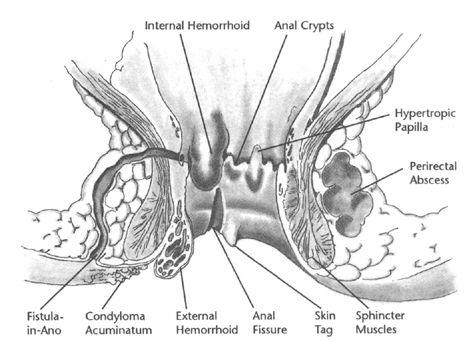
Figure 2.
1:
Benign Anorectal Disorders
Internal hemorrhoids originate inside the rectum and are covered by the colon lining (mucosa).
As they enlarge, they
can prolapse (hang) out of the anal opening.
When they stick out, they resemble small cherries.
External hemorrhoids, on the other hand, are enlarged veins covered with skin originating in and around the anus.
They are always on the outside, and although you may be tempted, they should not be pushed in.
Most people have a combination of both types of hemorrhoids:
an external component covered with skin leading into the internal portion covered with colonic mucosa.
External hemorrhoids create intense pain when they swell because of nerve irritation in their outer skin covering.
The swelling results when blood that normally flows through these veins clots inside them.
When blood clots, it causes intense inflammation, and you feel a swollen, hard, and very tender lump just beside your anus.
If you bend over far enough and get a good look at your hemorrhoid, it usually looks like a concord grape.
Its blue color results from the blood clot within the vein.
You may be wondering how you can see your hemorrhoids or anything else that is bothering you “back there.”
Of course, it is best to have a physician or partner look, but if you are too embarrassed, try a mirror.
Place the mirror on the floor between your feet.
Squat down over it in a well-lighted area and gently spread your buttocks.
Usually you’ll have to place your fingers quite close to your opening to spread your cheeks far enough apart for a close look.
Often hemorrhoids will look much smaller than they feel.
Thrombosed (clotted) external hemorrhoids do not bleed unless the clot causes so much pressure that it breaks through the skin.
Although this sounds frightening, the bleeding is usually minimal and actually represents the body’s own attempt at healing itself by extruding the clot.
Once the clot passes, swelling subsides and so does pain.
If the clot does not push through the skin, the body slowly
dissolves it and reabsorbs the clot back into your bloodstream.
As more and more of the clot is reabsorbed, swelling and tenderness decrease.
Whether the clot is pushed out or dissolved, usually an external hemorrhoid is history within two to three weeks.
All that remains of this painful episode is a fleshy piece of skin (anal tag) at your anal opening … until it happens again.
When blood clots in a vein, the resulting inflammation leaves behind a damaged vein.
So, once you’ve had a thrombosed hemorrhoid, you are more likely to get it again—and it may be worse the second time around.
This is why most physicians advise complete excision (removal) of a thrombosed hemorrhoid as soon as it occurs.
Although technically a surgical procedure, most often it is performed right in the doctor’s office with local anesthesia.
While some pain is associated with any surgery, in this instance the pain usually is less than what you experienced from the thrombosed hemorrhoid.
In the past, treatment of thrombosed hemorrhoids involved making a small incision into the hemorrhoid and removing the clot.
You may encounter a physician today who still recommends this “old” form of therapy, but I advise against it, because a simple “incision and drainage” does not remove the diseased veins, only the clot.
Although you will certainly feel better after the clot is removed, your chance of a recurrence is very great.
Most surgeons now recommend a complete removal of a hemorrhoid the first time a thrombosis occurs.
Men often wonder why they developed a thrombosed hemorrhoid in the first place.
It occurs when normal blood flow through a vein becomes disturbed and begins to clot.
Although anal sex can cause clotting, it is not likely to be the cause.
Most often hemorrhoids result from bearing down to lift something heavy or pushing out a hard bowel
movement.
Occasionally something as simple as a cough or sneeze will do it.
In most instances you will never know why you got the hemorrhoid.
Although internal hemorrhoids often have an associated external component, they are very different from each other.
Internal hemorrhoids are not covered with skin, and as such, they lack nerves that sense pain.
While rarely painful, internal hemorrhoids bleed when inflamed.
Hard stool rubbing against them creates a tear, or they burst from the pressure of a bowel movement.
If you notice painless bleeding after a bowel movement, chances are great that you’ve got an internal hemorrhoid.
Even though painless rectal bleeding is usually from a hemorrhoid, it should never be ignored.
I urge you to see a physician if bleeding persists.
It can be a symptom of something serious, such as a colon cancer.
In order to prevent hemorrhoids or treat the ones you already have, it is helpful to first understand their causes.
Anything that increases pressure in your anorectal canal will predispose you to hemorrhoids.
Straining during a bowel movement is the most common cause of increased pressure.
When you sit on the toilet and push hard to pass a stool, you force blood into your hemorrhoids and they swell.
The more you push, the more they swell, until, like a balloon that has been blown up one time too many, they no longer collapse back to their normal size.
Sitting on a toilet for too long also gives you hemorrhoids.
The longer you sit with your anus suspended over that grand canyon of your toilet, the more gravity pulls at the veins there and they swell.
So sit down, do what you have to do, and get up.
The bathroom is not the place to read
War and Peace.
If it is the only spot where you can be left alone to read, then put a chair in a closet, hang a good light there, and lock the door.
You may be back in the closet, but at least you’re less likely to get hemorrhoids.
If you’re sitting on the toilet unable to go, get up, walk around, and don’t sit back down until you feel the urge again.
Not only will walking help prevent hemorrhoids, it will also stimulate colonic motility and, with it, a bowel movement.
Internal hemorrhoids are not caused by anal sex, but it can certainly irritate them and cause bleeding.
(Use your imagination.
) If hemorrhoids are a problem and you want to have anal sex, choose a water-soluble lubricant, make sure your partner is gentle, and try lying on your stomach, a position that will decrease vein swelling.
Hemorrhoids can certainly make you miserable, but if you follow a few simple steps, you probably can avoid surgery.
First and foremost, keep your bowel movements soft but formed.
Diarrhea can be more irritating than a hard stool.
I usually advise patients to try to achieve one soft bowel movement a day.
Of course, this is not always appropriate for everyone.
Some people naturally go every other or every third day.
What is normal for your body is fine, as long as your stool is not hard when it finally passes.
The opposite is also true.
Some men (especially those on protease inhibitors) have more than one bowel movement a day.
That is fine, too, as long as their stool is soft and
formed.
